Digital Business Models For Health Insurance
 |
| Digital Business Models |
A business model describes the resources, processes and cost assumptions that an organization makes that will lead to the delivery of a unique value proposition to a customer.
Digital And Connected healthcare
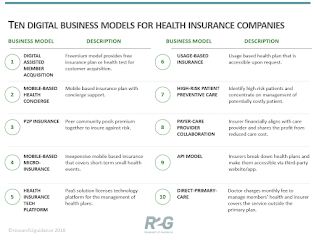
Ten digital business models for health insurance
- Digital
assisted member acquisition
- Mobile based
health concierge
- P2P
Insurance
- Mobile based
micro insurance
- Health
insurance tech platform
- Usage based
insurance
- High risk
patient preventive care
- Payer care
provider collaboration
- API Model
- Direct primary care
Digital technologies will transform the health insurance business and early adopters have started to implement new digital business models with initial success, according to a new Research2Guidance report. The report reveals new digital models are changing the way the insurers interact with patients.
For example, digital insurers have reworked the trust equation with the patient, outsourced much of their value chain to their members, and now know much more about them. Digital business models tend to also blur the lines between payer and caregiver organizations. Some of the first-movers already crossed the line and started to offer services which have previously been provided exclusively by doctors and nurses.
The ten disruptive digital business models that will transform the health insurance business are defined as follows:
1. Digitally assisted member acquisition is a freemium business model concept.
2. Mobile health concierge is a business approach designed for members to complete all health insurance tasks using mobile phones with the support from a concierge team.
3. Peer-to-peer (P2P) insurance refers to a risk-sharing community.
4. Mobile micro-insurance refers to the health insurance plans that cover short-term small health events or minimal ongoing health insurance.
5. Health insurers tech platforms license their technology for the management of health plans and members to their customers.
6. On-demand insurance is a usage-based model that enables members to access desired health plans upon request with the help of a mobile app.
7. High-risk patient preventive care model concentrates on insuring and managing potentially costly patient groups.
8. The payer & provider collaboration model stands for a closer, digitally enabled partnership between payers and care providers, especially hospitals.
9. The API health insurance model uses a list of pre-defined health insurance products accessible to websites and app providers via an application programming interface (API).
10. Direct primary care model. Within this model, a care provider or a hospital act like a health insurance company using a monthly subscription model.
Advantages of a Network Management System:
There are innumerable benefits in developing a
robust healthcare provider network management system. Below are some specifics:
●
Easy and quick access to numerous
options for healthcare
●
Increased affordability toward
health care provision
●
Leading edge in current and
emerging markets
●
Greater transparency in pricing
●
Higher quality of service
A robust healthcare provider network management system enables:
●
Mobility toward caregiving
●
Connects the ecosystem of clinics,
doctors, hospitals and patients
●
Creates a functional platform for
new models
●
Safeguards patient information and
data
●
Enables high quality data exchange
through mobile platforms
THE GROWING CHALLENGES
●
Increased Human Error
●
Payment Challenges
●
Security Issues
●
Increased Waste
●
Treatment Unpredictability
●
Limited Data Access
Business Process Automation
Government Intervention and Regulations
Healthcare Document Management Automation
Health Information Exchanges (HIE)
IoT Automation System Development
AI-Driven Healthcare Automation
HOSPITAL MANAGEMENT AUTOMATION
Fragmentation,
●
disseminated data repository ,high
manual processes and time delays are the issues faced without automation.
●
Enterprise-wide integration of all
networks into a single entity and provide high level of automation.
●
It aids hospital administrators in
improving operational control and streamlining operations.
●
Clinical pathways mapping improve
better diagnosis with good decision support system.
●
Web-enabled customizable solutions
includes patient administration, automated results capture, integrated billing
etc.
REVENUE CYCLE MANAGEMENT
●
To assist in adopting high-quality
electronic billing and payment systems with reduced coding errors
●
Standalone personalized medical
enrollment and billing platform for all healthcare providers.
●
Commercial built-in RCM with
content platform for streamlined reconciliation and increased audit controls.
●
Integrated transitions among the
health information systems and business practices across billing offices
●
Advanced data mining cum dashboard
reporting to analyse remittance and payer issues.
AUTOMATED MEDICAL RECORDS- EHR/EMR/PHR
●
OSP Labs develop HIPAA compliant
EHR / EMR / PHR application software with robust network & secure database.
●
Integration with evidence-based
tools, reliable patient portal and intuitive graphical for desktop and mobile
devices.
●
E-health point solutions utilize
technology to reduce complications, coordination of treatment, and efficient
delivery.
●
With each solution, insurance
payers & can innovate clinical management by improving efficiency and
patient outcome.
Each solution can be integrated independently, or with other point solutions.